Understanding How to Better Support Oncology Nurses in Conducting Advanced Care Planning in BC’s Cancer Care System
Lead: Heather Kilgour
Advanced Care Planning (ACP) is a process where patients reflect on what matters most to them and determine who may make decisions for them should they be unable to speak for themselves.
Background
Advanced Care Planning (ACP) may include reflecting on personal values and beliefs, naming a substitute decision maker, sharing preferences about goals of care with family, friends, or healthcare workers, and recording personal wishes via documents such as an advanced directive or a letter to their loved ones. The benefits of ACP have been well-established, including decreased anxiety and depression towards end-of-life, increased satisfaction with care, and care that aligns with patients’ goals and preferences. Despite the known benefits of ACP, healthcare provider engagement in ACP is low, and ACP has not been integrated into standard nursing practice at BC Cancer.
As a nurse at BC Cancer, Heather Kilgour recognized the opportunity to improve ACP practices and create more supportive environments for oncology nurses to conduct ACP. An important first step was to gather more information related to the current ACP climate across BC Cancer, barriers and facilitators to engaging in ACP, and changes needed to better support oncology nurses to conduct ACP.
Purpose
The purpose of this study was to (1) understand oncology nurses' experiences and perspectives related to ACP and (2) inform how to better support oncology nurses in engaging in meaningful ACP discussions across BC’s cancer care system.
Study
In this study, we invited registered nurses, licensed practical nurses, nurse practitioners, and nursing leaders across BC Cancer and Community Oncology Network sites to participate in semi-structured interviews. During the interviews we asked open-ended questions to better understand nurses’ perspectives and experiences related to ACP, including what changes nurses perceived are needed to feel supported in engaging in ACP with their patients.

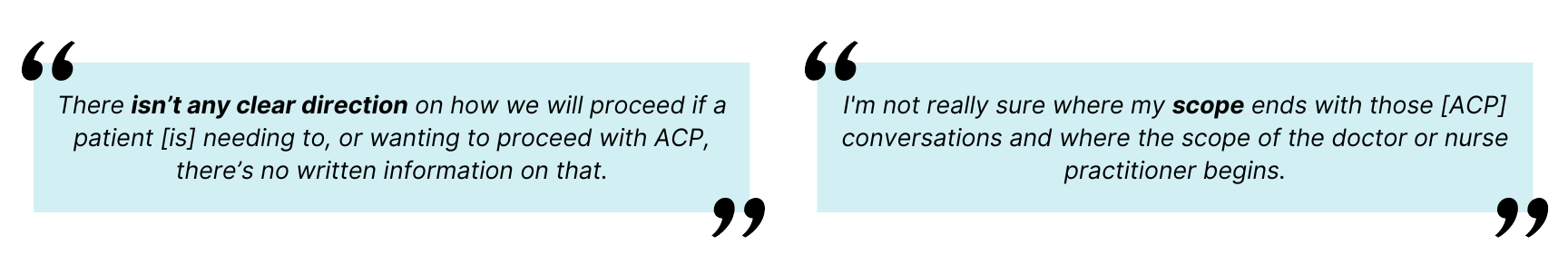
Barriers of ACP 1. Uncertainties related to the nursing role in advance care planning and how nurse ought to engage Oncology nurses identified several uncertainties related to ACP in oncology nursing practice, including how and when a nurse ought to engage, and role delineation in ACP across disciplines. These uncertainties were compounded by the absence of a clear organizational workflow outlining ACP-related practices.
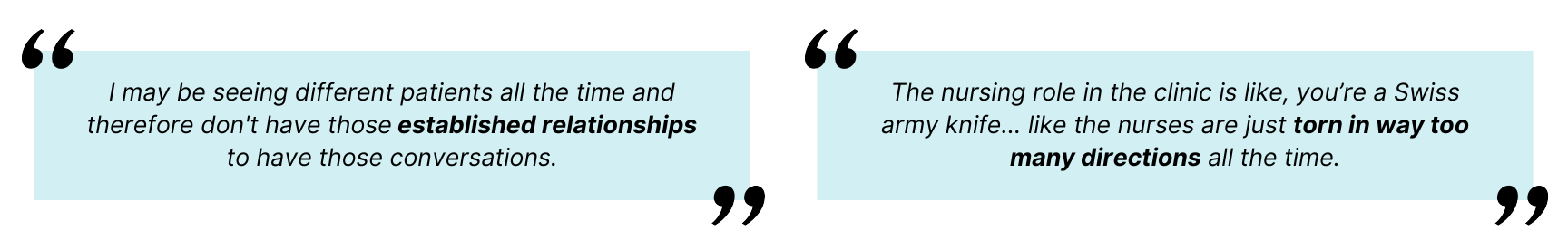
2. Structural barriers, a lack of time and space, challenges with continuity of care within nursing practice and interdisciplinary team dynamics Lack of time, space, and privacy to hold ACP conversations with patients and their families; challenges with continuity in nursing care that inhibit nurses from establishing longitudinal relationships with patients; and team dynamics that prevent interdisciplinary collaboration when approaching ACP.
|
Changes Needed Oncology nurses identified ACP-related uncertainties and advocated for a clear and cohesive organizational approach, integrated and ongoing educational pathway, and dedicated time for advance care planning. They emphasized the need for a team-based approach that facilitates trust and communication between nurses, patients, and interdisciplinary colleagues. |
Learn More
Read more about the next step of our plan -> ACP Knowledge Mobilization
If you’re interested in learning more about this project please contact Heather Kilgour at heather.kilgour@bccancer.bc.ca.
BC Cancer Foundation is the fundraising partner of BC Cancer, which includes BC Cancer Research. Together with our donors, we are changing cancer outcomes for British Columbians by funding innovative research and personalized treatment and care.